ACLS tachycardia algorithm: Managing stable tachycardia
Last updated: June 27, 2023
Version control: Our ACLS, PALS & BLS courses follow 2020 American Heart Association Guidelines for CPR and ECC. American Heart Association guidelines are updated every five years. If you are reading this page after December 2025, please contact support@ACLS.net for an update. Version 2021.01.c
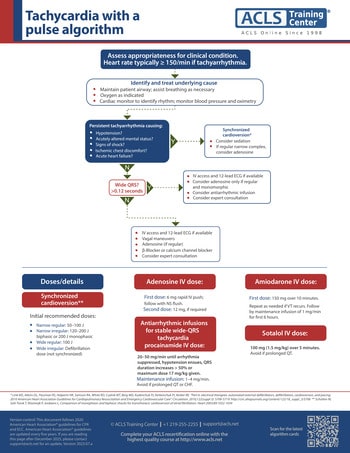
For tachycardia, assess appropriateness for clinical considering and treating the underlying cause. Tachycardia is heart rate over 150 beats per minute. Maintain a patent airway and assist breathing as necessary. Administer oxygen if hypoxic. Place the patient on a cardiac monitor to identify rhythm and monitor blood pressure and oximetry.
Persistent tachycardia can cause hypotension, acutely altered mental status, signs of shock, ischemic chest discomfort, and acute heart failure. If the patient is having any of these signs consider emergent synchronized cardioversion, follow your manufacturer's guidelines. Consider sedation prior to cardioversion but do not delay treatment. If the rhythm is regular with narrow complexes, consider adenosine 6 mg IV rapid push.
If the patient is stable, measure the QRS. If QRS is wider than 0.12 seconds, establish IV access and obtain a 12 lead ECG. Consider adenosine only if the rhythm is regular and monomorphic. Consider antiarrhythmic infusions such as procainamide, amiodarone, or sotalol IV. Consider an expert consultation.
If QRS is less than 0.12 seconds, establish IV and obtain 12 lead ECG. If the rhythm is regular, encourage the patient to try a vagal maneuver. Give adenosine 6 mg IV rapid push if the rhythm is regular. Consider a beta blocker or calcium channel blocker and seek expert consultation.
For synchronized cardioversion, follow your manufacturer’s guidelines. Initial recommended doses for a narrow regular rhythm is 50–100 Joules. For narrow irregular rhythm use 120–200 Joules. For a wide and regular rhythm use 100 Joules. For a wide irregular rhythm use immediate defibrillation.
Adenosine is given as a rapid IV push. First dose is 6 mg followed by a normal saline flush. If a second dose is required, give 12 mg IV rapid push.
Antiarrhythmic infusions for a stable wide-QRS consider Procainamide, Amiodaone or Sotalol IV. Procainamide dose is 20–50 mg/min until the arrhythmia is suppressed, the patient becomes hypotensive, the QRS duration increases more than 50% or the maximum dose of 17 mg/kg is reached. Followed by a maintenance infusion of 1–4 mg/min. Avoid Procainamide if QT is prolonged or the patient has signs of heart failure. Amiodarone is given as a first dose of 150 mg over 10 minutes. Repeat as needed if VT recurs. Follow by a maintenance infusion of 1 mg/min for the first 6 hours. Sotalol is given 100 mg (1.5 mg/kg) over 5 minutes. Avoid if the patient has a prolonged QT.
Planning to certify/recertify ACLS?
Get a reminder when you need to take the exam

Written by Jessica Munoz DPN, RN, CEN, providing nurse training at Yale New Haven Health-Bridgeport Hospital since 2022. Previously in healthcare and education at Griffin Hospital, St. Vincent's College of Nursing and Sacred Heart University Medical Center.
More by this author: